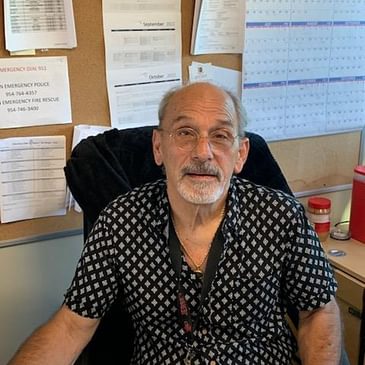
When you hear the words "health policy", what comes to mind? A dry, barren desert? Not for John Silver, a nurse who has dedicated decades of his life to studying it and believes it’s anything but dry and lacking in substance. He was so passionate about understanding it that he left nursing to pursue a Ph.D. in comparative studies. He serves as President of the organization, Nurses Transforming Healthcare, whose mission is to transform healthcare into a model based on wellness and disease prevention, driven by nurses, which is affordable and accessible to all. John believes we as nurses need to remember our social roots as a profession in order to affect change. The goal is ambitious, yet gaining momentum every day. I have no doubt with our collective power, John and the masterminds behind NTH will radically change healthcare. I teased him about being a deep thinker, but honestly, a world without deep thinkers would just be boring. In the five-minute snippet: Vintage guys rule! For John's bio and book recommendations, see links below!
John's book list
Nurses Transforming Healthcare
Once a Nurse, Always a Nurse podcast
Publications:
Completing the Circle of Nursing
An Open Letter to My Fellow Americans
Nursing Declaration of Independence
Contact The Conversing Nurse podcast
Instagram: https://www.instagram.com/theconversingnursepodcast/
Website: https://theconversingnursepodcast.com
Give me feedback! Leave me a review! https://theconversingnursepodcast.com/leave-me-a-review
Would you like to be a guest on my podcast? Pitch me! https://theconversingnursepodcast.com/intake-form
Check out my guests' book recommendations! https://bookshop.org/shop/theconversingnursepodcast
Email: theconversingnursepodcast@gmail.com
Thank you and I'll see you soon!
[00:00] Michelle: When you hear the words health policy, what comes to mind? A dry, barren desert? Well, not for John Silver, a nurse who has dedicated decades of his life to studying it and believes it's anything but dry and lacking in substance. He was so passionate about understanding it that he left nursing to pursue a PhD in comparative studies. He serves as president of the organization nurses transforming Healthcare, whose mission is to transform healthcare into a model based on wellness and disease prevention, driven by nurses, which is affordable and accessible to all. John believes we as nurses need to remember our social roots as a profession in order to affect change. The goal is ambitious, yet gaining momentum every day. I have no doubt with our collective power, john and the masterminds behind Nth will radically change healthcare. I teased him about being a deep thinker, but honestly, a world without deep thinkers would just be boring. In the five minute snippet, vintage guys rule. Here is Dr. John Silver. You're listening to the conversing nurse podcast. I'm Michelle, your host. And this is where together we explore the nursing profession one conversation at a time. Well. Hi, John. Welcome to the podcast.
[01:35] John: Hello, I'm back. It's great to be here.
[01:38] Michelle: Yes. Technology is wonderful, isn't it?
[01:42] John: And it's sometimes right when it works.
[01:47] Michelle: Yes. Well, thank you so much for joining me again. I really appreciate it. I'm excited to talk to you because, first of all, you have a lot to say, and we need to get the word out. The other reason is you're just so interesting. You're a deep thinker, and I can't quite relate to a lot of the deep thinking, but it strains my brain and it helps me grow, and so it's just such a worthy endeavor. And I met you on LinkedIn, and I've met a lot of wonderful, great people on LinkedIn, and so I know that you are going to be another one of those great people. So just excited for a lot of reasons today.
[02:35] John: Thanks. Well, go live in a cave for 20 years, and you don't have any choice but to be a deep thinker.
[02:41] Michelle: Oh, my gosh. And you have a sense of humor, too. It's a dry sense of humor, which I relate to because my brother Chris, he's like, you very deep thinker, very dry sense of humor. So I've known that all my life. And we'll get to Chris in a little bit, but you have a really interesting path to where you are today. So do you want to just start by telling us how you got here?
[03:09] John: Well, I'm old, so I'll make it kind of brief. I started in healthcare in 1974. Never thought about healthcare before that. My first job was a security guard, but I fell in love with what was going on around me, and they hired me, and I did orderly and Er tech and then EKG tech, and then 1978, a respiratory therapist. Finally 1984 my RN. And I spent the next pretty much two decades, went to three states. I was a critical care nurse. I worked agency nights because that's where the money was and just kind of minded my own business. When I came back to Florida in the decided to go back to school, get my bachelor's, and I met a lot of nurses that were coming back for their bachelor's, and they were all kind of complaining the same thing nursing had been complaining about for 1520 years. So I started getting kind of interested in why nursing couldn't control its own practice domain in the hospitals. This was right as the California nurses were making their movement towards staffing ratios. So I did a master's degree, and the school let me kind of create my own master's program, even though it was in nursing. And I kind of crafted it along the lines of health policy. And I got to go up and work with George Mason's health policy institute over a summer. I did two internships in Washington. I came back and worked with a rep in Florida. And I was kind of thinking at that time it was know, people just don't understand what nursing does. So I did a master's thesis on proactive media utilization, how you use cheap, affordable media to not just get your word out, but also for some kind of political change so you could get the support from the public and other people for what you were advocating for. So when I finished my master's, I started really seeing a lot as an Er nurse at that time of problems in the healthcare system writ large. And I'd known there were problems, but I hadn't really focused a lot on what they were. So I started getting kind of really consumed by these two questions why can't nursing control its own practice domains? Except now that also included why NPS couldn't get independent practice and prescriptive authority across the board in the US. And then the second question was, what's wrong with healthcare, and how do we fix this? So I read a lot, and I didn't really see many answers coming out from my discipline nursing. I didn't really see anything coming out of public health, certainly nothing coming out of medicine or the industry itself. And so they just opened a brand new PhD program at my school called the public intellectual PhD in comparative studies. And so I thought, you know, I'm going to step completely out of healthcare, go into a multidisciplinary PhD, and look back at healthcare historically, contextually, socially, blah, blah, blah, blah, blah, and see if I could find a solution, maybe some kind of system design that might work a lot better than what we're doing now. So that's what I did.
[06:38] Michelle: You literally grew up in healthcare, in the whole healthcare industry, and you've gone from the very beginning to where you are now a PhD RN. And that's really impressive. And you are the president of an organization called Nurses Transforming Healthcare. You guys are doing some really great things. And you do have an instagram, and I'm following you guys. You are working with three women, so there's four of you, is that right?
[07:16] John: Well, we're bigger and bigger and bigger all the time. We're up to kind of like eight or nine regular attendees at the meetings that are engaged with the specific activities of our Nurses Transforming Healthcare
group. We're up to, I think, 150 or 200 supporters.
[07:34] Michelle: Okay, that's really great. And I went on there and I did donate. So it's something that I would encourage other nurses and healthcare professionals to do because this work is really important. And I have to admit I don't know a lot about health policy. It's always been kind of a dry subject and you probably hear this a lot, but health policy drives so much of what we do. Why do you think nurses are not involved more in health policy?
[08:11] John: Well, I think it's a couple of things. One is we really don't have a professional organization that's very savvy or empowered to really do anything politically. The major organization we have, of course, is the American Nurses Association, but they represent only about really over 4% of the nurses in the US. And when you go into Congress, one of the things congressional people will look at is not just who your organization is, but how much strength they have and support. If all of nurses supported the Ana, we'd have over 4 million members. We don't. And they know that socially, too. Nurses are very disparate. We're kind of all over the place from all cultures and ethnicities and social groups. And a lot of nurses, after you put in a couple of twelve hour shifts, you really don't want to think much about health policy.
[09:14] Michelle: That's so true.
[09:16] John: And you got kids to worry about and social lives and all that stuff. And I think we've also kind of become accustomed almost like an oppressed group that we really don't have any power to bring to the table. We don't want to be marching in the streets with Red Berets, which it's kind of that union wing of nursing, that kind of theoretical approach we're really in. A lot of us work in very small markets and we really can't afford to be politically aggressive and then be fired. And then the next hospital is 15 miles away you got to go to yeah. So we're kind of isolated. We don't have any communication method with all of us. There's no real newsletter that goes out to all the nurses in the country. So it's been very challenging to try to reach out.
[10:17] Michelle: Yeah, I mean, all those things that you said are true and those are all things that we can work on so that we can communicate better. I'm definitely going to get your organization in touch with the nursing beat. Last month, I interviewed the CEO, Tamara Al Yasin, and the COO, Hana Burns, and they have a newsletter that goes out to it's over 22,000 subscribers right now, and it's just growing every day, and it goes out five days a week. And we need to get nurses transforming healthcare in there because it's just going to reach so many more nurses. And like I said before, you guys have so many great messages. I'll get you in touch with them.
[11:08] John: That'd be great. I tell people this all the time. If only 10% of the nurses would listen to what we're saying and agree with it and support us, we'd be the largest nursing organization in the world. So we're not asking I don't have any expectation if 4 million people are going to join our I mean, it'd be great if they would, but there's no membership fee to join. We're an umbrella organization. We're trying to bring groups and nurses and other people. It's going to take all of us to do this kind of under the umbrella, listen to the system design I'm proposing, see if it makes sense, and if you can support it, great. Any donations go to our operational costs. Kathleen Bartholomew is a nurse culture expert. She's one of my team members, or one of the founders, I should say. Kim Evans, who's an integrative nurse practitioner in Kentucky. She's owned her own practice for over 20 years. She's also a key founder, leanne Myers, who ran a podcast called Once a Nurse. Some people may have heard that, and we have other key members too, but none of us are salaried. We're not trying to make money out of this. Just we came together, agreeing on the ideas and then said, enough of just talking. How can we get something done?
[12:30] Michelle: Yeah, I listened to Leanne's podcast the other day, a few episodes, and it's really good. I was really impressed. And I'll definitely put that link in the show notes, as well as the link to your website, which is nursestransforminghealthcare.org. But one of the things that I read, one of your publications, is completing the Circle of Nursing, and in it you talk about the seven goals to make US. Healthier as a nation. And I'm just going to go through those really briefly. So, number one, equitable targeted, data driven access appropriate to every community's needs. Number two, quality evidence based care. Three, equitable, targeted and evidence based distribution of resources. Four, interdisciplinary practitioner led administration so that the system is congruent with their values and maximizes their skill sets. Five, equitable and positive outcomes. Six, cost efficiency. And seven, social accountability and a mandate for direct public reporting. So where are we in the process of achieving either all seven or one or two of them?
[13:45] John: Well, those goals were actually the first thing I did, because when I decided to start to look back as a philosopher, I said, okay, so what are we trying to accomplish? What would the goals of or what should the goals of a healthcare system be? And it took a while, but I came up with those seven goals. Then I was at a bigger university than I am now, and I had the luxury of doing some travel. So I went down to Argentina and studied their health system. I went over to Berlin and gave a talk actually at a design conference about how you design a healthcare system.
[14:25] Michelle: Wow.
[14:27] John: While I was there for ten days, I studied the Bismarck model, the German system, how they did it. I went back two years later and talked to the First European STTI convention in Cardiff, Wales and met nurses from all over Europe. So I had great discussion time for days with nurses about what they thought of their health
system, what they thought of nursing. So I came back here and I kind of gathered all the system models I could find around the world, the coherent ones, mostly the OECD countries and some in Asia. And I kind of put them all on the table, including our system, and went through them one by one to see which ones met all seven goals. And none of them did. And in fact, our system didn't meet any of the seven goals. So I thought, okay, well, let me see if I can rethink what health care is. And I started thinking, if I think of healthcare as services that are delivered to communities, as opposed to 500 million individual billable interactions with providers or facilities, it changes your perception of what health care could be. The quintessential problem in healthcare philosophically was we were not willing to decide whether health care was a right or a privilege in this country. A lot of countries made that decision, said it was a right. We have not done that. So I thought all know I'm going to ask U. S. History. There had to have been something in our history that emerged that was too important socially to be left to just a commodity market. But we weren't willing to call it a right. And I found the electrical issue in the 20s, so I'm sure most people are familiar with electricity, but we didn't always have it. And when it started emerging in cities around the country, it was privately owned. There were multiple LLC corporations out of it. They charged whatever money they wanted and they ran it to whoever they wanted, basically people that could afford it. And they didn't distribute that to other communities that they couldn't afford it. And they certainly weren't going to run 60 miles of wiring out to rural areas. But a lot of the US. Economy was changing at that time, and manufacturers were starting to come out with all this electrical stuff, dishwashers and washing machines and things that people wanted. So in 1935, FDR stepped in and they passed the Public Utility Holding Corporation Act. And they basically restructured the electrical industry into a public utility. So I thought, oh, it's public utility. So I brought public utility model forward and I put it on the table with the goals. And I found out if I change how it's administered, because the typical public utility has political appointees and all that stuff in there. And I changed how it's financed because it can't just be user based financing. I found out this model takes healthcare right down to the street in every community. It becomes an obligation of the system to provide services wherever they're needed. So I had to redesign the administrative system and again, the financing. And that's kind of where that started.
[18:08] Michelle: Well, it's brilliant. When I first read about it, I just was blown away because it's so logical and it's so doable that I can't believe it hasn't been done yet. I can't believe that no one to this point has had that idea.
[18:31] John: Well, that's not quite fair. There was a doctor group in the 90s that came out, but they didn't do the diligence of changing that administrative structure and they couldn't figure out the financing for it. And then there was another group that came well after me five, six years ago, and they were also kind of locked in, seeing that the model itself would work, but they couldn't figure out how to finance it or administer it to make it work. But the article you were talking about completing, the Circle of Nursing, is not really I mean, it introduces the public utility model, but that's not actually what the article is about. The article was we need to, as nurses, get back to what our mission should be. We were designed to be a socially active force, not to know, hiding away in long term care facilities and hospitals. Nursing as a profession came out of people like Dorothea Dix, who I know she wasn't a nurse, please don't write me, but she came out of social activism. And in her particular case, it was the insane asylums in New England. And then we had people know Mary Seacole that showed a different type of path for nursing, where we actually go to where we're needed. We don't wait for things to be brought to us. It's the old story. I don't know if you've heard about the doctors and nurses on the river and they're pulling all these dead, wounded and injured people out of the river. And they do this for years. One day the nurses just start packing and leaving, and the doctors come over and go, hey, what are you doing? We need you here. The nurses said, we're going upstream to find out who's throwing all these people in the river. So it's that kind of approach. But if we're going to be a socially active force, we ourselves have to be a socially active force. So in completing the circle of nursing, I'm talking about, for example, a hurricane reaches its full potential when the wind bands wrap around the eye. The nursing eye is our code of ethics, our mission to serve, our willingness to go out and find people that need help and help them. The wind bands are things like the nurse practitioners and the RNS and the LPNs. But to me, it's got to be even bigger than that. It's got to be the home care aides. It's got to be even people in their own homes that are taking care of sick people, of community health workers. We're all kind of part of that nursing family, and we should be that family because that's how we're going to become the socially active force that will kind of restore our integrity and drive as a profession. I don't know if that makes any sense to anybody but me, but it makes perfect sense.
[21:33] Michelle: And do you think we're on the precipice of nurses becoming more socially active? Because I've seen a lot in the last year, two years, about nurses getting fed up and leaving the profession and nurses striking. So do you think that we're about to make a huge shift?
[21:59] John: Well, what I don't see is the vision any of these groups have for what they want at the end. I mean, we understand basic issues like staffing ratios. Yes, that should be national. This is absurd. But to do that and fight these little battles facility by facility and state after state is a monumental task to me. It's always been smarter to fight a war than a series of endless battles. So to me, the issue is to go public with an actual vision of a nursing in the sense of caring for community, caring for where people are trying to help people, vision of what this healthcare system could look like. And the whole goal of Nth nurses transforming healthcare is to get
empowered enough to take the commercials that I've already written and get them produced and in some markets around the country to start having the American public understand blue and red healthcare impacts all of us, that what we have now is sucking money out of communities. We're paying way too much for all this stuff. And to be honest, we're getting lousy outcomes in most areas. Maternal health is collapsing. Black maternal health is a global embarrassment. Public health, our lifespan is decreasing. The cost of everything is going up. This is an unsustainable model. And if we don't have a clear vision of how we want to change this, I think we're going to be in trouble. And it's just going to fragment out because it is going to collapse.
[23:54] Michelle: Yeah, I was really saddened the other night when I was listening to the debate, the first Republican debate, and nowhere was health care brought up at all. That was not an issue on the table. And I understand it was just the first debate. And hopefully it will be an issue for both parties, but it's not on our radar yet. We all need it. We all participate in it. We all want it.
[24:27] John: The problem politically is the Republicans. And I try to be as neutral as I can because to me, health policy is apolitical. But the Republican Party at large has no vision for anything they want to do except get rid of Obamacare. I get it. They want to destroy that legacy and bring down the Patient Protection and Affordable Care Act. But I would doubt any of them have even read it and know what the PPACA was all about. And if you actually read it, it was a feeble, but a really good attempt to start moving forward with design issues in healthcare that we need to get going. The Democrats for their side are kind of locked in a two way fight. The big one, of course, is Medicare for all is what some of the more progressive people want. The trouble with Medicare for all is it doesn't solve the problems in healthcare. It's another attempt like HMOs and ACOs and value based care and managed care and direct primary care and value based care and all these other schemes to work at the insurance level, but it doesn't change the structural problems that we have in the healthcare system delivery system. And then the only other option they have, which CMS seems to have adopted, is a 20 or 30 year vision for incrementally improving the Patient Protection and Affordable Care Act. Well, the problem with that is people are dying now. We don't have 20 or 30 years to sit around while some scheme of Medicare Advantage or value based care or whatever they want to call the scheme of the week to kick in and hopefully show some effects. So that's kind of where we sit politically.
[26:25] Michelle: Well, on the State of Reform website, you did a piece for them, and it was titled A Nurse's Vision to Transform the Healthcare System. And in that, you talked about your proposal to reorganize the current healthcare structure from a predominantly fee for service model to regionally based systems that use data from public university health centers to drive the best healthcare solutions for their particular communities. So my question is, with your public utility model, what happens to me if I'm living in a sick community? And I was reading that, like, five of the sickest communities in the US. Are. Montgomery. Alabama. Augusta. Georgia. Columbus. Georgia. Shreveport. Louisiana. Brownsville. Texas. So if I'm living in those cities that are on the sickest cities in America list, do I have to pay more for my health care? Since it's regionally based, how would it work?
[27:34] John: Do you pay more for electricity in that community than you do in the rich area of the city? Okay, so the idea of the administration portion and the financing of the health care for the administrative portion we live in a federated republic, so we kind of have to respect the balance of federal government, state government. At the same time, health care is a concern for everybody. It's a national concern. It's a national security concern. If you look at statistics, for example, of people that volunteered after 911 to go into the military and something like 65% were rejected because of health, obesity, diabetes, all these kind of chronic conditions that we suffer from in this country, well, that kind of makes it a national security issue. States are paying way too much. 20% of their budgets are more in some states for health care services. The facilities in and of themselves will not make the effort to go out to these distal communities. And even when we have seen some efforts, for example, Mayo Clinic in Minnesota a year or so ago, they withdrew that initiative of providing health services into rural communities. And of course, the overarching problem is we're insurance driven, which means and profit driven. So if the facilities don't see a profit going out, they're not going to invest the resources in nursing. We should have learned that lesson back in the 70s when there was a ton of research coming out about how you deliver maternal services and primary care services to rural communities. We just couldn't get anybody to pay for it. So the idea is we all pay. Corporations now are paying something like 24, $26,000 a year per employee. What I'm talking that down to is $1,000 per employee. And they don't have to provide any health insurance because we're not going to need health insurance anymore. A smaller business might pay if they can afford it based on profitability, $500 an employee or $200 an employee. Smaller businesses may pay 25 or $50 per employee. Cities, you're still going to pay some money, but well over half of what they're paying now. The same thing for states. And then as individuals, since the health care system is there for us, we will also pay like in a utility bill, maybe $50 a month. But you won't have to buy health insurance, and you won't have any copays or deductibles, and you won't have to pay any hospital expenses if you have emergency surgeries or something. Now, the idea of the state based regions. Well, first there's a central council that sits in Washington. It's affiliated, but not under HHS and NIH and CDC, and it's also affiliated with Congress, but not under Congress. And they're actually going to interact with all of those bodies and then disseminate information out to the state based regions. On the flip side, the state based regions are going to report back to them on best practices that they're
finding when they see results so that that information becomes available to all the state based regions. These state based regions are no longer competitive. So I house each state based region in a university medical center, or if they only have one, I guess, in another full service large hospital and they're connected with the academic disciplines at the universities. They sit on this council. I have nursing as the chair of the council. But medicine is there, EMS is there, public health is there community representation, all for that part of their state based region. Their obligation is to go out and find out what these communities need and then figure out how to deliver that service to them in a cost efficient manner. So basically, they'd be budgeted for the provision of healthcare services to their regions.
[32:10] Michelle: So it sounds like there's going to be a lot of extra money kind of floating around because employers are going to be paying a lot less. There's not going to be insurance premiums because insurance companies are going to be no more. So where are we going to put all that money back into the system, into the public utility model? Or what are we going to do with that?
[32:35] John: Well, that generation of income from everybody will pay for the state based regions they'll be budgeted. The money that your corporation is now spending on you should go to you. A lot of people don't understand that. They think their company is just paying this out of gratuity. No, they're paying you less so that they can pay you this benefit. So hopefully they'd be able to pay you more. At the same time, they won't have to have an infrastructure in and of themselves to supervise the health insurance and the health insurance process for each of their employees. So that's another reduction in cost for the corporations. The cities and states will no longer have to be doing outreach services to the rural areas and all this kind of low income housing health services and all this because the system should be looking at every community to decide what they need and then figuring out the way to bring that there in a cost efficient manner. The figuring out part kind of confuses some people. Well, I've said for a long time you empower nurse practitioners and nurses to deliver health services. You can pretty much just get out of our way because we're going to go in and do it.
[34:05] Michelle: Yeah, nurses are like that. We're go getters we see a problem and we want to solve it and we find the answers. So I think we're the perfect profession to spearhead something like this. One of the really interesting quotes that I saw in one of your pieces that you said was innovating in a dysfunctional health system doesn't change the system. And I was like, yes. Can I get an amen? Because it's just so obvious and so profound at the same time. And I've interviewed several nurse innovators on this program and it looks like nurse innovators are either innovating to leave the bedside or leave the profession altogether. Do you think that we are innovating ourselves out of the nursing profession?
[35:07] John: Well, I think they're catch words disrupting and innovating and all. Of this. They're not talking about systemic reform, which is what we need. So they're saying basically, we give up. There's nothing we can do about health care, so let's go see if we can find some other way to make money. I would rather we come together and fix the problem.
[35:29] Michelle: Yeah, that's always the best solution. Come together and fix the problem. And like I said before, nurses are good at doing that. We take it as a challenge and it's definitely a worthy challenge. There's nobody better to do it?
[35:48] John: No. We're the most trusted profession in the country.
[35:51] Michelle: That's right.
[35:54] John: Read our code of ethics and I bring this up all the time. There's nothing in there that says we're going to go make ourselves the greatest egg in the nest. It's not about us.
[36:06] Michelle: About us.
[36:07] John: It's about what we can do for the other.
[36:10] Michelle: I mean, that's the basis of nursing. That's always been like, we don't do it for the applause. Right, right. Yeah. Well, I wanted to touch on to another great publication of yours, and these are all going to be linked. So this was an open letter to my fellow Americans, and I'll just start by reading this small part of what you wrote. So all of this points to a healthcare system that is globally dysfunctional, poorly distributed, and not delivering the quality of care which the American public expects from the three plus trillion dollars being spent yearly. We have failed as well, socially and politically, to address the major issue. Is health care a right or a privilege? How can we possibly decide what to do to address the major healthcare system design issues without having a meta paradigm to work with? And then you ask the question, how can you possibly know what road to take when you don't know where you're trying to go? And so the part that really made me chuckle was that I interviewed my brother Chris Patty in episode four, and he's a doctorally prepared nurse researcher and the director of research at his institution, and he actually taught health policy at the university level. So, like I said, he's a deep thinker like you, John. And we were discussing Florence Nightingale's book notes on Nursing, what it is and what it is not. And Chris said, I honestly have yet to run into a nurse that could tell me the American Nurses Association definition of nursing, and then went on to say exactly what you said. How do you know you're doing it right if you don't know what it is you're doing? And if you can't explain it to people, particularly people who aren't nurses, how do you expect anyone to understand it, value it and support?
[38:08] John: Yeah, if you look at the vision of the American Nurses Association, it's a healthy world through the power of nursing. I don't even know what that means. How are we going to make a healthy world? The vision
that I set forward for us as nursing was to lead an integrated, holistic wellness centered healthcare system that addresses the needs of all our communities right there in your face. And our mission is to become the independent, socially active force america needs to achieve that. So we're a little bit different in our approach of what we think nursing should be doing.
[38:52] Michelle: Well, you've said over and over again you've asked this question, why can't nursing control its practice domains? What do you mean by this?
[39:03] John: Well, the essential problem in most facilities is that nursing is overhead. So if you're running a business, you try to keep your overhead as low as possible. I actually took an administrative job for six months. I knew they get rid of me quick as a director because I wanted to peek behind the curtain and see there was kind of two things. One, I was an Er nurse at that same facility for a while, and I couldn't understand why we couldn't get patients moved out of the emergency room, particularly after, like, 06:00. And so it was basically putting a cork in the emergency room at our busiest time. And then all of a sudden, at midnight, all of these beds opened up and we started moving patients up to the floors. And I couldn't understand kind of why that was happening. So when I took over the director, the first thing I tried to do was cut down. So my day nurses coming into these busy telemetry floors I ran four telemetry units, would only start with five patients. Well, as you can imagine, that went over with a dull thud with administration. But I started going to the staffing office every night before I left to make sure that they were staffed appropriately for the day before. And part of the reason I did that was they would frequently pull our PCAs off the floors to go sit with, like, Baker Act patients or something. And so my staff would come in, only have two PCAs for 40 patients and seven or eight patients to start with. That's ridiculous. Yeah, we had a high acuity floors. So anyway, I started doing that funny. I got called in one day to the CNO office, and I got taken over to the CFO's office, and the CEO was there. Generally not a good sign, by the way. And the CFO sat me down to explain the matrix. And the matrix was a staffing matrix where really the only bedcount that mattered was the 12:00 census, midnight census. So they'd keep admissions in the Er, so they didn't have to admit them in as patients until after midnight so they could staff the day shift with a lower number. Then we're probably going to be wow. And that was kind of eye opening to me. Anyway, I refused to acknowledge it, kept doing what I doing. And after a couple of days, they called me into the Seattle's office with the head of HR. No, that's even a worse signal, by the way. And they told know this was unsustainable.
[41:52] Michelle: Wow.
[41:52] John: The ironic thing is a week later I started at another hospital as an Er nurse with the same corporation. So I guess I didn't leave with a black mark.
[42:02] Michelle: That's crazy. Wow. And I remember that. I remember doing acuities and staffing and the schedule and man, that hearkens back to a really crazy time. So talk a little bit about another piece of yours, the nursing Declaration of Independence. And I will link that as well. But I thought that was really great too.
[42:35] John: Well, some people find that a little combative, but I'm a little hostile when I think of how many people need help and how impotent we are to deliver services that are needed. So I wrote that actually 20 some years ago and I copied the Declaration of Independence from the United States. I just kind of made it about healthcare and nursing. And the idea was to declare our independence from being servants to other forces within healthcare, particularly, of course, medicine, but also hospital administrators or anybody else the reasons why we did it and then what we were going to do once we got our independence. So in the case of the American Republic, it was taxation without representation. Well, what I'm talking about is employment without representation, a profession without representation. And I think Americans would acknowledge, even though I would still argue that a lot of people do not understand the critical role we play until of course they're admitted and see what we do. So part of that's too going to be explaining a little bit about what nursing is and what it does.
[43:57] Michelle: Yeah, one of the lines that came from that was whereas nursing has lost its philosophical bearing in health care and lost touch with its socially active roots in practice due to the systemic design, do you think that nurses are aware of our socially active roots? Do you think we know where we came from? And do you think if we did, it would change the way we feel or it would motivate us to be more socially active?
[44:30] John: Well, I think all of us as nurses going through our schooling read something about the history maybe we read know, Florence Nightingale and Clara Barton and Lillian Wall, but there were just kind of names we memorized for a test. We thought of them as kind of like Fred Flintstones of nursing, but really they were the initial creators of what our potential was and they weren't restrained by medical practice acts in that day. So it wasn't like they know, fearful of medicine coming in and doing something. To me, my personal hero, the one whose picture sits on the wall of my office, is Lillian Wald. I think her vision of nurses going out into communities to deliver health services to tenement buildings, to migrants, to whoever needed help, but also the understanding that healthy communities are much more than just how many cases of this you have or how many cases of that you have. She also addressed community health and got food carts regulated so people weren't getting poisoned when they stopped and ate something and created backyard play areas and communities for kids so they weren't getting run over in the streets. Her vision was much bigger than just us taking a service to a person and delivering it. It was an understanding of community. And I talked to CMMI a couple of weeks ago, and I was trying to get them to understand this, that a healthy community is much more
than just a hospitalization rate 30 miles away at a closest hospital. And making a healthier community is much more than just reducing that by 25%. I use more of the World Health Organization understanding of a healthy community. It has to have a sense of optimism, of potential, of not being abandoned by the rest of society, of having access to things that other people in society have internet and remote schooling and all the potential things we can do with technology so that people living 80 miles away from a city don't feel like they're living in 1953 when everybody else is living in 2023.
[47:08] Michelle: Yeah. Yours is definitely more holistic approach.
[47:14] John: Well, we're a holistic profession.
[47:15] Michelle: It's true. Yeah. And interestingly. So I'm doing a piece right now on Mary Carson Breckenridge and all of her work with the Frontier Nursing Service and doing exactly that, going out into these remote parts of the state and delivering care and reducing infant mortality and maternal mortality almost down to zero. And I didn't learn of her until really about six months ago. And I've been a nurse for 36 years. So I think we need to learn more about where we came from in order to figure out where we're going.
[48:04] John: Yeah. These early nurses up until the 1920s, but you said Frontier nursing still continues. These women were riding burrows, motorcycles and horses and walking into these remote areas to try to deliver help to people. I mean, my God, how much more of a motivated profession do you want?
[48:29] Michelle: Exactly.
[48:31] John: And now we've got nurse practitioners and we've got nurses, and we understand that we need partners, and we can ally ourselves with pharmacists and physical therapists and nutritionists and whatever that community really needs education in based on. And here's another part I had to write or come up with. I am not in favor, really, of public health community assessments. They're too allopathic for me. To me, 95% of what we're talking about here is all nursing care. So why aren't we doing nursing assessments of communities? So, fortunately, I have an old contact of mine, Gene Watson, University of Colorado, and a student of hers, I think it was in Canada, published an article on the Watson Caring Community Assessment community Assessment Tool. So I looked at that and I said, man, this is, like, perfect. So I took that and I combined it with some of the World Health Organization community assessment process and came up with basically a nursing focused community assessment that would really result in almost like a nursing care plan for this community.
[49:50] Michelle: That's genius. Yeah, it's funny. Our institution, gosh, this was 25 years ago, probably we adopted Gene Watson's theory of caring, and that was the first time ever in my career that I had heard of a nursing know it's. I feel like this is more the norm than it is the exception in nursing. And I don't think it was something back then, 25 years ago. I think it's still happening today. I think if you took 100 nurses and lined them up and said, who's your favorite nursing theorist? Probably 90 of them would say, or Florence Nightingale, right? Gosh yeah. I feel like we have a long way to go.
[50:52] John: Well, I'm old enough that I actually walked when talked with Madeline Linenger. I've heard Gene Watson talk. We emailed back and forth many times in the went to a caring based school. My dean was Anne Boynkin, also out of caring theory. I actually had dinner one night with Patricia Benner.
[51:14] Michelle: Oh, my gosh.
[51:16] John: I've met a lot of these imaging king. I knew Imogene king. I've had a lot of fortunate events where I've met a lot of the theorists, but most of the theorists were mid level theorists. There's never really been a macro theory of nursing or grand theory of nursing, so I tried to write one of those, too.
[51:43] Michelle: That's what I was going to say.
[51:44] John: You've got to come up with, no, I never published it.
[51:49] Michelle: You haven't published it yet?
[51:52] John: Actually, I don't publish much because the times I tried in the always got back these denial letters saying, oh, well, we're a journal that's not that political, or, we don't want to offend anybody.
[52:06] Michelle: Wow.
[52:07] John: Of course, most of them depend on advertising money. The few times I was published, it'd be this big disclaimer over the top of know, basically, hey, this is just this one nut nurse in Florida. We have nothing to do with it.
[52:21] Michelle: Oh, my gosh. Well, do you ever feel like you're swimming upstream, like, with your efforts? What keeps you going? What motivates you?
[52:32] John: No, I actually feel like I'm really engaged with this. I have a lot of optimism. I think that at some point, enough nurses are going to want to start thinking about, hey, I really love this work, working with people. I want to keep being able to do it, and I don't want to spend the rest of my life giving enemas to somebody for $40 or whatever else people are doing. Ive infusions or all the other things. I tell you, I worked in hospitals for years. I loved it.
[53:10] Michelle: Same.
[53:11] John: Not a problem. I was definitely an alpha adrenaline junkie, er trauma, burn units. I loved it. All I felt valuable. I felt important, but not to the system.
[53:25] Michelle: That's a good distinction to make. Is nurses transforming healthcare working with any legislative know, any congresspeople, any senators?
[53:42] John: We were working with some legislators in Minnesota. They had a big surplus of money there. I don't know how long ago. It was a year or two ago. And we got actually introduced to a bill I told you earlier about the Mayo Clinic backing out of those rural communities. And our offer was to set up a know, give us two of these rural communities, set up a budget, and we'll show you how independent practicing nurse practitioners can go in, assess the community, and you come back in. A year. And you're going to see a healthier community, and you're going to see people that trust their healthcare providers that are coming in. And it got all the way up to one of the sessions, and then one Republican gentleman came up, and he was convinced we were trying to open the door to single payer, which of course we didn't. He said, I went to your website. I think it's single payer. Well, you obviously didn't go to our website, because I say right there, I'm not in favor of single payer. So you didn't read anything. And the other lady was married to a doctor, also a Republican legislator. And she wanted to know where the medical supervision was for the nurse practitioners. And I told her, well, we told her, look, you passed independent practice three years ago. I don't know how you define independent practice, but I define it as not needing oversight. So they shot it down. Those two people shot it down and was never passed. But we are working with a small community in Texas. This was a kind of neglected community. And we did a very subtle walk in, not deliberately, kind of accidentally. And we have somebody now working, a nurse practitioner and also a registered nurse, working with this community to provide nutrition and healthcare education. The nurse practitioner is our partner. She designed an app for community people that when they need something, they can look on the app, and if they need a ride somewhere, which is frequently a problem. Rural communities is people don't go to health follow up stuff because they either can't afford it or they don't have access to a ride to drive there. And then community members can build up points for assisting their neighbors. And this is going so well that when we went in to do the community assessment tool, the people in the community said, listen, there's areas you don't want to go into in this city. We'll do the assessment for you.
[56:27] Michelle: Wow.
[56:28] John: So we've had a lot of buy in in this, and we're seeing some really good results. And of course, the Anecdotal stories are amazing. And hopefully we'll have that published sometimes at the end of the year so where we can get in. We will get in. Yeah.
[56:48] Michelle: Well, do you think you'll see a major shift in your lifetime?
[56:56] John: Well, I definitely hope so. I'm counting on the next year or so.
[57:00] Michelle: That's awesome.
[57:01] John: I think we're reaching a critical mass. If if we could just get that grant come in or the financial support we need to kind of get this off the road. I think once we're able to hit the national media with this vision of what health care should be and could be and explain the benefits, I think it's a system Americans understand. The farmer in the remote area that goes in and turns his morning light on in the kitchen, doesn't shake his fist at the sky screaming, you damn socialists. Every time he turns on a light.
[57:37] Michelle: Right.
[57:38] John: It's a system model Americans understand. It's worked really well until we started corrupting it in the 70s with a lot of political nonsense and privatization efforts. So it's a model Americans understand. They should accept it reasonably well. And I think it's politically fairly simple to do well.
[58:03] Michelle: I think it's brilliant, and I think you're brilliant, and I just wish you so much luck in your endeavors. And I encourage nurses to go to your website. Nursestransforminghealthcare.org, become a member, donate, read what you're all about. Go to your LinkedIn. It's amazing. You can read all of your publications there and just really get involved and become aware of what's going on and what needs to happen. What changes need to happen. So thank you, John, so much for coming on. I just I've learned so much, and I know that you've brought just a ton of value to my audience. So thank you so much for that.
[59:01] John: Thank you for having me on. Michelle. It's been a great pleasure. And anybody that wants to please come to our site, join us, come to our meetings. We're pretty open. Donate, if you yeah.
[59:16] Michelle: Yes, I second that. Well, you know, it's time to play the five minute snippet, because that's what we do at the Know. Our audience gets to see the off duty side of Dr. John Silver. So are you ready to play the five minute snippet?
[59:34] John: Rutrow? We better get ready.
[59:38] Michelle: All right. I will set my timer. So some of these are would you rathers so would you rather be a skyscraper window washer or a dog walker for 24 hours?
[59:54] John: Dog walker.
[59:56] Michelle: Okay. Do you have a fear of heights?
[59:59] John: No, but I have a lot of respect for him.
[01:00:04] Michelle: Enough said. Okay. What's a surefire way to grab your attention?
[01:00:13] John: I think ask an intelligent question.
[01:00:17] Michelle: That's great. Yeah. You're going into your deep thinking mode again. Would you rather have song with good lyrics or good music?
[01:00:32] John: Probably good music, because that's what sticks in your head.
[01:00:38] Michelle: Right? Like that earworm that's there all day.
[01:00:41] John: Yeah, exactly.
[01:00:43] Michelle: What's the top thing on your bucket list?
[01:00:48] John: Fixing health care.
[01:00:50] Michelle: Wow. Okay. That's worthy. Would you rather always be right or always get the last laugh?
[01:01:02] John: I don't think anybody's always right, and I don't really laugh at people, so I don't know. Halfway in between, I guess.
[01:01:13] Michelle: Okay, that's fair.
[01:01:16] John: There is vindication in talking to somebody for months, and this has happened a couple of times with some systems theorists and economists and stuff where I've talked to them for two, three months, and finally they'll say, you know, John, you're yeah, there is some vindication in that.
[01:01:36] Michelle: That feels huh?
[01:01:38] John: Yeah.
[01:01:40] Michelle: Is there anything that you keep on your desk that kind of boosts your mood?
[01:01:46] John: My desk or your workspace? No, a couple of favorite books, but that's about it.
[01:01:56] Michelle: Oh, you're going to have to give me those book recommendations.
[01:01:58] John: Pictures of my son.
[01:02:00] Michelle: Okay. Family. Yes. So would you rather take part in an experimental transplant or uncertain holistic remedies?
[01:02:14] John: I guess that depends on the problem, but I think I'd rather take a chance with the holistic remedies.
[01:02:23] Michelle: Okay, let's see. What is something vintage that you love?
[01:02:31] John: Everything I have is vintage.
[01:02:34] Michelle: You're like? Define vintage.
[01:02:37] John: Well, how about over 2000 years old?
[01:02:40] Michelle: Oh, okay. Yeah.
[01:02:42] John: I have a necklace I wear, and the centerpiece of that necklace is a coin that was dug up from Pompeii.
[01:02:51] Michelle: Oh, my gosh. I love old coins.
[01:02:54] John: Probably be worth a lot more now than it was when it got covered with volcanic ash.
[01:02:59] Michelle: Yeah. Wow. That is something to really treasure.
[01:03:04] John: I love that piece.
[01:03:05] Michelle: I want to see a picture of it. You have to send it to me. Okay. Would you rather have 365 days of snow or unrelenting heat?
[01:03:19] John: Heat.
[01:03:21] Michelle: Well, why did I think you were going to say that? You live in Florida?
[01:03:25] John: Live in Florida? Yes. Cold to me is where you go when you want to go skiing.
[01:03:32] Michelle: Okay. Yeah. I don't know, I was just like with this question, I said, I think I'd rather have snow because I live in a very hot place right now. All right, this is the last one. What's the best present you ever received?
[01:03:52] John: Wow, the best present. Honestly, when I was ten years old, I was living in Chile. My father was stationed down there, and I was living in Chile, and it was really difficult for them to get any kind of presents. And he bought me this airplane, a Stuka fighter jet that you flew around in circles on a string and control. It had a gas engine. The string was like 30, 40ft long. You could fly it in circles. And I had more fun with that stupid plane than I think I've had fun with anything my whole life.
[01:04:38] Michelle: It sounds wonderful. What a great memory and a great gift. And you have certainly brought your gifts today, and I just appreciate you so much. John, thank you so much for coming on.
[01:04:53] John: You're very kind. Thank you. And come on, nurses, come help us.
[01:04:58] Michelle: That's right. Again, I'll put all that in the show notes, but go to nursestransforminghealthcare.org and become a member. Donate and just find out what the mission is.
[01:05:11] John: Yes.
[01:05:12] Michelle: All right. Well, you take care. Have a great day.
[01:05:16] John: Thank you very much. It's been a pleasure.
[01:05:18] Michelle: Same here's. It.